Though it is an important organ, do you need your pancreas to live? The pancreas is part of the digestive system and plays a vital role in blood sugar levels. Despite its essential role, certain conditions may require the removal of this organ. While this is a dramatic and life-changing shift, with advances in modern medicine it is not impossible or life-threatening with the proper care.
Do You Need Your Pancreas To Live? FAQs About the Pancreas
It is challenging for many patients to understand how removing a vital organ is possible or how they can survive without it. Some organs, such as the spleen, appendix, and gall bladder, are removable with little consequence. Still other organs, such as lungs and kidneys, are removable but will affect a patient’s quality of life. Which category does the pancreas fall into?
What Is the Pancreas, and What Does It Do?
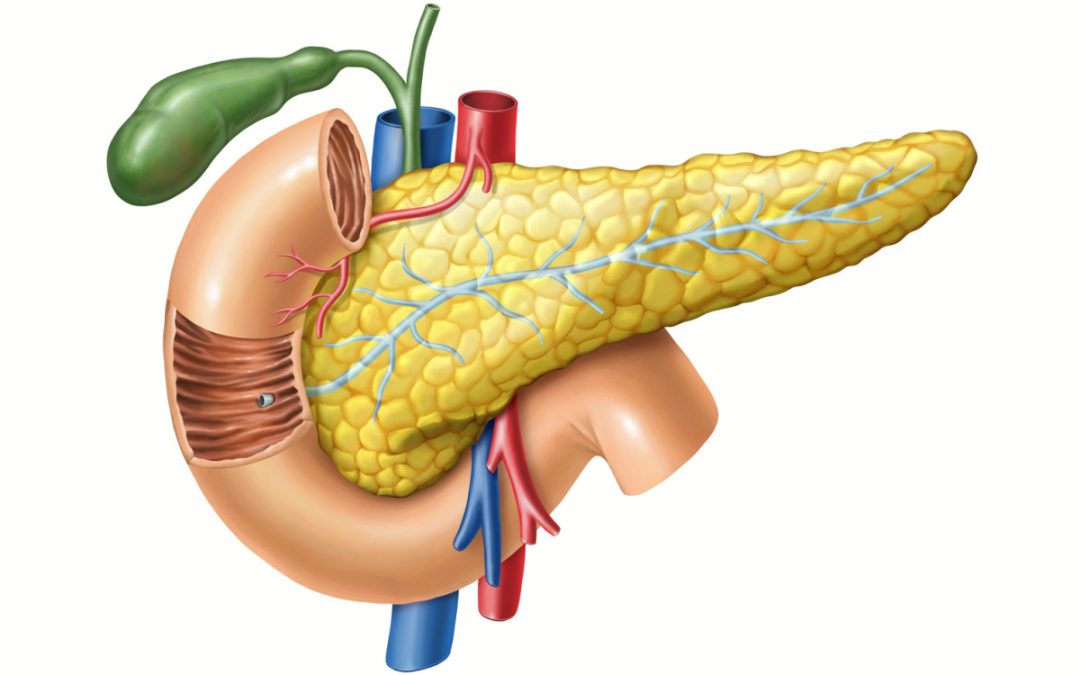
The pancreas is a long, leaf-shaped internal organ that sits deep in the abdominal region between the spine and stomach. Technically, it is a gland, meaning it secretes chemicals crucial to biological function.
The pancreas has two primary jobs: blood sugar regulation and digestive enzyme production. Insulin, the main product of the gland, helps to maintain healthy blood sugar levels. If the pancreas does not produce an adequate insulin supply, blood glucose can become dangerously high because the body cannot absorb it fast enough. It also hinders the body’s ability to use glucose from food, resulting in malnutrition or other health issues.
Digestive juices or pancreatic enzymes are also a product of the pancreas. These juices help the body break down and absorb nutrients and food waste. Pancreatic production of digestive enzymes occurs in the exocrine part of the pancreas, while insulin creation occurs in the endocrine portion of the organ.
While hormones enter directly into the bloodstream from the pancreas, the digestive enzymes flow through the pancreatic duct to the duodenum — a portion of the small intestine. In the digestive process, the pancreas works in tandem with the liver and gallbladder, producing various enzymes to aid in the digestion and absorption of food.
Can You Live Without Your Pancreas?
Do you need your pancreas to live? Decades ago, problems with your pancreas were generally fatal, but with medical advancements and further understanding, it is now possible to live without a pancreas. In fact, depending on the reasons for the removal, patients can live a relatively normal life.
A pancreatectomy is the surgery for pancreas removal, and it can be partial or complete. A partial removal eliminates the damaged part of the pancreas and leaves the other part functional, reducing adaptations for patients.
A complete pancreatectomy is the removal of the entire pancreas. Patients undergoing this operation automatically develop diabetes upon its completion, requiring insulin injections for the rest of their lives. Also, the surgery may include removing parts of the stomach, small intestine, and bile duct.
Removing the pancreas can also inhibit the body’s ability to absorb nutrients and adequately digest food. Patients will need artificial digestive enzymes to replace the natural enzymes of the pancreas.
Therefore, while it is possible to survive without a pancreas, patients must commit to lifestyle changes and consistent injections of insulin and enzymes. The transition is challenging but possible, and survival rates are promising. Consult an internist with Arizona Premier Surgery to learn more.
What Happens After a Pancreas Removal?
Patients typically require medication and lifestyle changes following a complete pancreas removal. In rare instances, a transplant might be necessary.
Medications like insulin and artificial enzymes help replicate the products of the pancreas, ensuring your body can function and absorb nutrients as usual. The enzymes come in a pill form that patients take before meals to help digestion.
The insulin a doctor prescribes depends on the specific condition of the patient. In most cases, patients are put on long-acting and fast-acting insulin. Together, each mimics normal pancreatic function. Typically, patients will take between one and four shots daily, doling out small doses during the day and larger doses after meals.
A partial pancreatectomy also requires some supplementation, but the amount depends on the health and functionality of the remaining pancreas. Some patients who have normal function before surgery and lose up to two-thirds of their pancreas during the procedure may still have relatively regular insulin and enzyme production from the remaining gland.
Adopting necessary lifestyle changes can also affect treatment and wellness following a pancreatectomy. Patients must create a habit of checking blood sugar levels and planning their diets.
As a diabetic, which all complete pancreatectomy patients become, watching carb and sugar intake is vital, as is remembering insulin injections and medications. Some treatments are forgiving, permitting an occasional lapse or forgotten pill, but routine neglect is life-threatening.
Routinely forgetting insulin injections can result in blindness, heart attack, kidney failure, nerve damage, or stroke. Forgetting enzyme pills can result in vitamin deficiencies that cause gastrointestinal issues or lead to osteoporosis.
Why Won’t Surgeons Always Remove Your Pancreas If You Have Cancer?
A pancreatectomy is a possible treatment for pancreatic cancer, but it is not always a curative option. Pancreatic cancer is a challenge for early diagnosis because symptoms are not always apparent, which is why many people refer to the disease as a silent illness. When symptoms occur and doctors make a diagnosis, most patients have locally advanced or metastatic disease, meaning a pancreatectomy is an unsuitable treatment option.
Still, a pancreatectomy is an option for the right type of cancer and a timely diagnosis. Depending on the cancer’s stage, size, and spread, a surgeon may recommend removing the spleen, gall bladder, nearby lymph nodes, common bile duct, and parts of the stomach and small intestine.
Consult the Medical Professionals at Arizona Premier Surgery About Living Without Your Pancreas
The pancreas plays an essential role in the body, but do you need your pancreas to live? If you adhere to medical instructions, take the correct medications and injections, and adopt necessary lifestyle changes, you can survive without a pancreas. For more information, contact the medical professionals at Arizona Premier Surgery and schedule a consultation.
Sources:
https://www.medicalnewstoday.com/articles/319521#recovery-and-lifestyle-changes
https://fg.bmj.com/content/13/e1/e88
https://www.healthline.com/health/can-you-live-without-a-pancreas
https://utswmed.org/medblog/living-without-a-pancreas/
https://integrisok.com/resources/on-your-health/2022/september/can-you-live-without-a-pancreas
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9005876/
https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P00682